Discussions of the upcoming 5G technology sometimes focus on whether or not the millimeter-wave frequencies involved can damage human life. What gets less press is that radio frequency energy in other bands can be therapeutic. It can be useful to review a few of these uses to understand the beneficial role RF energy can play.
One such use is called radio-frequency ablation (RFA). RFA uses frequencies that extend from 350 to 500 kHz. The point of RFA is to cause extremely localized heating of tissue but not so much heating that tissue becomes vaporized.
As a medical procedure, RFA consists of applying medium-frequency ac current to the heart or to other kinds of dysfunctional tissue. Using a needle-like RF probe, the RF energy can be precisely introduced into a cancerous tumor, causing a temperature rise that shrinks or destroys the dysfunctional tumor without harming nearby healthy tissue. Similarly, highly localized heat can be accurately placed to treat a variety of other pathological conditions without creating significant collateral damage.
These procedures are generally performed in conjunction with image guidance such as X-ray screening, CT scanning or ultrasound. All of this requires thousands of dollars in medical equipment, but the procedures are quick and efficient, compared to older X-ray therapy, and they often take place on an out-patient basis so the cost per treatment is constrained.
Other applications are in dermatology, treatment of varicose veins, obstructive sleep apnea therapy and pain management. Lower back pain responds well when RF energy is applied to heat specific nerves, stopping their ability to transmit signals to the brain. One successful therapy is to identify nerves to be ablated by means of local anesthesia, providing temporary relief. Then RFA is applied to the nerves that responded well to the injections. This can be done on an out-patient basis without use of general anesthesia, thereby avoiding associated risks and expense.
Other areas in which RFA is an effective therapy are RF lesioning, to close veins where intrusive surgery is not feasible due to trauma and in liver resection to control bleeding.
Readers familiar with microwave ovens might wonder why, if heating is the goal, RFA doesn’t use frequencies closer to the 2.4 GHz radiation of these kitchen appliances.
It’s possible to employ microwave frequencies (and ultrasonic frequencies) for RFA, but they are not widely used. The main reason is that RFA evolved from electrosurgery devices used mainly for cutting or coagulation-type procedures. The electrosurgery equipment uses essentially the same type of RF generators and frequency range as RFA. This prior experience simplified the regulatory approval of RFA devices at these frequencies.
Nevertheless, research continues on RFA-type treatments at frequencies outside the 450 kHz area. One recent study found that the electrical resistivity of tumor tissue is significantly lower than that of normal tissue at lower frequencies, where tumor tissue has approximately half the resistivity of normal tissue. Preliminary studies suggest this difference between normal and cancer tissue in the frequency range below 100 kHz may be exploited to preferentially heat tumor tissue.
Many of today’s RFA instruments have electrodes that are designed to be inserted via endoscopes. So the electrodes are necessarily quite thin. They also typically have a bipolar design where the RF current is applied to the patient via a pair of similarly-sized conductors. The RF electrical current oscillates between the two conductors, heating the intervening tissue by the synchronous oscillation of intracellular ions.
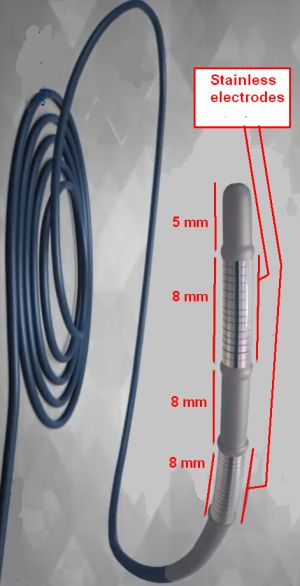
An example is the Habib Endo HPB (from EMcision Ltd. in the UK) which is a single-use, bipolar device designed for RFA of malignant bile ducts and to ablate tissue growth after the placement of metal stents in bile ducts. The device probe has a 180-cm working length, which can be deployed through an endoscope of at least 3.2 mm diameter. At the tip of the probe are two circumferential, 8-mm-long stainless-steel electrodes separated 8 mm apart. Ablation procedures with the device use about 10 W of 400-kHz power applied for up to two minutes, followed by a one-minute resting period.
One can surmise that the design of the electrodes for this device is nontrivial. Consider that the most efficient energy transfer for RF transmissions takes place for antenna dimensions that are an integral fraction of a wavelength, usually a quarter-wavelength. But a quarter wavelength at 400 kHz is about 615 ft, clearly not a dimension compatible with a probe small enough to fit in an endoscope. Thus the probe designers had to devise a matching network for the 8-mm electrodes that presents the 400 kHz generator with a circuit behaving as much as possible as a quarter-wave antenna. Additionally, the matching network design must be such that most of the 400 kHz energy gets delivered to the electrodes rather than to the matching-network components.

Leave a Reply
You must be logged in to post a comment.